Every State has a department or agency responsible for maintaining the integrity of its Medicaid programs and public health initiatives.
While the names of these enforcement authorities may vary—such as the Department of Medicaid or the Department of Health Care Services—they all are required to implement regulations regarding the ineligibility of providers who have been disciplined or have lost specific licensing privileges.
Why State Exclusion Lists when there is the OIG LEIE?
States are required to notify the Health and Human Services (HHS) Office of Inspector General (OIG) only when they exclude or terminate an individual or entity based on federal law.
States are not required to notify the OIG (nor should they) of actions based on State laws because if the sanction fails to meet the criteria for a federal exclusion, the exclusion will not be posted on the LEIE.
Plus, it can take several months for the OIG to process the State-reported sanction, determine whether it will also impose a federal exclusion based on a violation of federal laws, and post it to the LEIE.
For instance, a State might exclude a party for failing to pay State taxes or for a variety of other reasons that would not be valid bases for federal exclusion. For this reason, states maintain a list of individuals and entities who are terminated, suspended, sanctioned, or otherwise excluded from the State Medicaid program under State law.
States may also maintain their list as a central registry of State sanctions, including non-healthcare actions, as well as exclusions or terminations.
For example, federal exclusions can be imposed for failing to repay federal loans, and it would be reasonable for a State to have a similar exclusion basis.
Why do some States not have an Exclusion List?
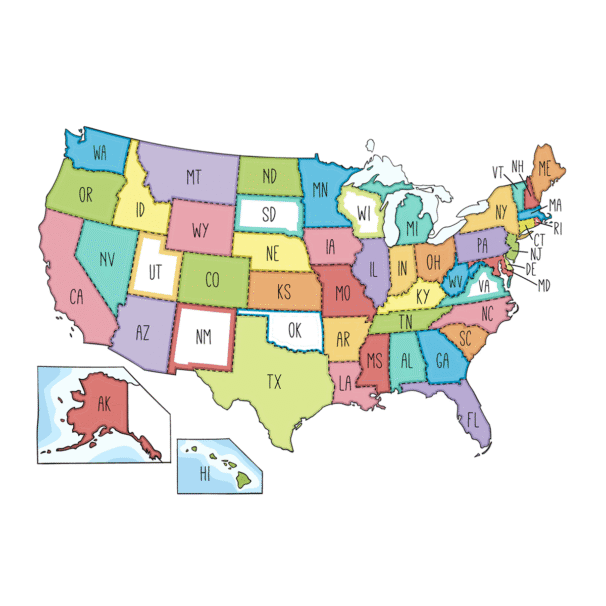
States aren’t required to maintain a State exclusion list, and seven states have elected not to: New Mexico, Oklahoma, Rhode Island, South Dakota, Utah, Virginia, and Wisconsin.
These states may have other sanction lists. For example, State agencies responsible for contracting may maintain a separate debarment list; the agency responsible for providing services to those in need of care may maintain a list of individuals who cannot participate; or the State Department of Health might maintain its own list, and so on.
How do OIG & State Exclusion Lists differ?
One difference is that some State lists don’t exclusively contain healthcare sanctions. They are a centralized list of several sanctions, each with a different impact.
This is similar to the System for Award Management (SAM) at SAM.gov, which includes debarments beyond healthcare.
The other, and more important, difference is that federal exclusion lists do not post State exclusions; therefore, the State list is where to find exclusions based on violations of State laws.
Do all State Exclusion Lists include the same information and format?
No.
You’d think we would have a standard for something this important, but sadly, no.
Unfortunately, each State that publishes an exclusion list has different formats and varying levels of detail.
Some lists are in Excel format, others are in Word or PDF, and some are simply HTML web pages.
Information available in State Exclusion Lists can also vary widely, with some that include little more than a name and address.
Why screen all State Exclusion Lists?
Section 6501 of the Affordable Care Act (ACA), “Termination of Provider Participation Under Medicaid if Terminated Under Medicare or Other State Plan”, requires State Medicaid programs and the Children’s Health Insurance Program (CHIP) to terminate the participation of any individual or entity that has been terminated from Medicare or any other State’s Medicaid program for cause.
This provision is intended to enhance program integrity by ensuring that federal funds do not reach providers excluded for serious offenses, such as fraud or abuse, regardless of the originating State’s termination.
There is no national list of State Medicaid program terminations. Although you may find some State Terminations in other State lists.
HealthProviders DB is a national database of all State Exclusion Lists. Exclusions are imported monthly as they become available, keeping the database up to date.
How frequent screen for exclusion?
According to the OIG’s Special Advisory Bulletin issued in May 2013, the OIG recommends that healthcare organizations check their employees and contractors against the LEIE monthly.
In addition, monthly screening is mandatory in at least fourteen States, while many others strongly suggest that providers screen employees and vendors against their State list and the LEIE monthly.
What are the regulatory requirements for exclusion screening?
Federal database checks — 42 CFR Part §455.436 regulations, all State Medicaid agencies must do all of the following:
(a) Confirm the identity and determine the exclusion status of providers and any person with an ownership or control interest or who is an agent or managing employee of the provider through routine checks of Federal databases.
(b) Check the Social Security Administration’s Death Master File, the National Plan and Provider Enumeration System (NPPES), the List of Excluded Individuals/Entities (LEIE), the System for Award Management (SAM) (formally the Excluded Parties List System (EPLS)), and any such other databases as the Secretary may prescribe.
(c)(1) Consult appropriate databases to confirm identity upon enrollment and re-enrollment; and
(c)(2) Check the LEIE and SAM (formerly the EPLS) no less frequently than monthly.
Who needs to be screened?
Healthcare organizations must screen new hires and regularly monitor current employees, as well as the individuals and entities with whom they do business, to avoid potential Civil Monetary Penalties.
This includes doctors, nurses, pharmacists, and other healthcare professionals interacting with patients and federal healthcare programs, such as Medicare or Medicaid.
Even if someone isn’t directly providing care, they might still be involved in billing, patient records, or managing payments from federal programs. These roles are critical, and OIG exclusion checks should apply here.
Think of anyone supplying medical equipment, pharmaceuticals, or services to a healthcare organization. Just because someone isn’t a full-time employee doesn’t mean they shouldn’t be checked. They must pass an OIG background check if they provide goods or services involving federal funds.
Volunteers can be involved in patient care or sensitive healthcare operations in specific settings. While not always required, screening volunteers can help ensure the organization maintains compliance with federal regulations.
Search HealthProviders DB
HealthProviders DB profiles include all Federal & State Exclusions, Terminations, Suspensions, Sanctions, and Debarments Lists, mapped as Exact or Possible matches, greatly simplifying your exclusion screening.
Exclusions that match by NPI number, or by full name and address, are Exact matches.
Exclusions are imported monthly as they become available, keeping the database up to date.
An individual or organization whose billing privileges have been revoked by the OIG or any State cannot participate in Medicaid, Medicare, or the Children’s Health Insurance Program (CHIP).
Enter an NPI number, license number, or provider name in the search field below to search the Exclusions.
Alternatively, you can also search the Providers.
Alaska – Alabama – Armed Forces Pacific – Arkansas – American Samoa – Arizona – California – Colorado – Connecticut – District of Columbia – Delaware – Florida – Federated States of Micronesia – Georgia – Guam – Hawaii – Iowa – Idaho – Illinois – Indiana – Kansas – Kentucky – Louisiana – Massachusetts – Maryland – Maine – Marshall Islands – Michigan – Minnesota – Missouri – Northern Mariana Islands – Mississippi – Montana – North Carolina – North Dakota – Nebraska – New Hampshire – New Jersey – New Mexico – Nevada – New York – Ohio – Oklahoma – Oregon – Pennsylvania – Puerto Rico – Palau – Rhode Island – South Carolina – South Dakota – Tennessee – Texas – Utah – Virginia – Virgin Islands – Vermont – Washington – Wisconsin – West Virginia – Wyoming
Select a State to view the list of Exclusions by State.
Additionally, you can narrow the list by city, among other options, from the Filter Panel, which you can open by clicking the vertical ellipses ⋮ in the upper right corner of the app.
Use HealthProviders DB Batch Exclusion Screening and Exclusion-monitoring Solutions to avoid potential Civil Monetary Penalties.