Explore clinicians who provide high-value/high-quality patient care.
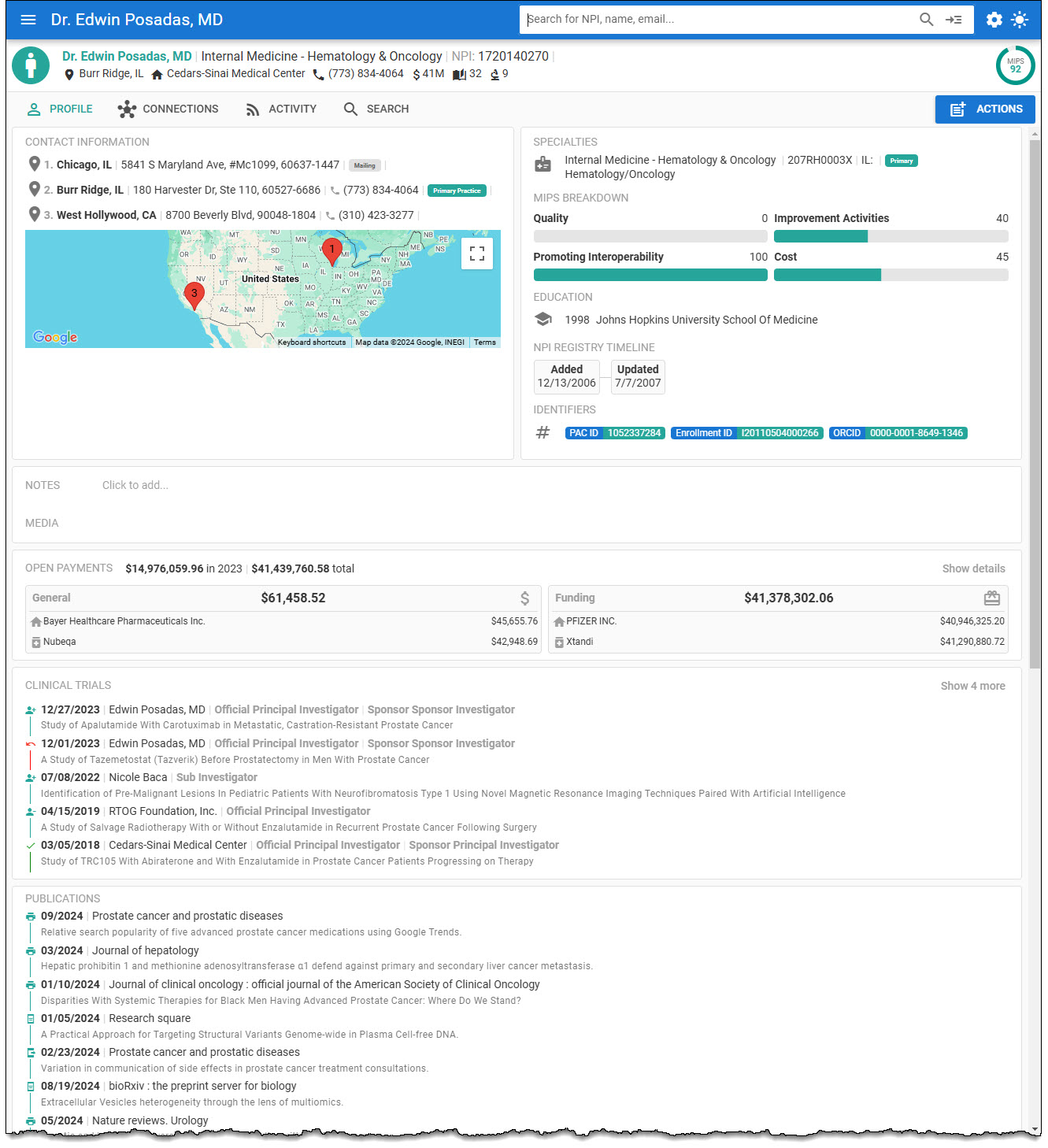
HealthProviders DB includes the Merit-based Incentive Payment System (MIPS) Scores from the Centers for Medicare & Medicaid Services (CMS).
The MIPS score evaluates healthcare providers’ performance and determines payment adjustments based on quality of care, cost efficiency, and the use of electronic health records.
About CMS MIPS Scoring
The Merit-based Incentive Payment System (MIPS), established by the Medicare Access and CHIP Reauthorization Act of 2015 (MACRA), came into effect on January 1, 2017. It is a significant catalyst for transforming the healthcare industry from fee-for-service to pay-for-value.
MACRA ended the Sustainable Growth Rate (SGR) formula, which would have resulted in a significant cut to payment rates for clinicians participating in Medicare. In response to MACRA, the Centers for Medicare & Medicaid Services (CMS) created a federally mandated Medicare program, the Quality Payment Program (QPP), to improve patient care and outcomes while managing the costs of services patients receive.
Clinicians providing high-value/high-quality patient care are rewarded through Medicare payment increases, while clinicians not meeting performance standards have a reduction in Medicare payments.
Clinicians may participate in the QPP in one of two ways:
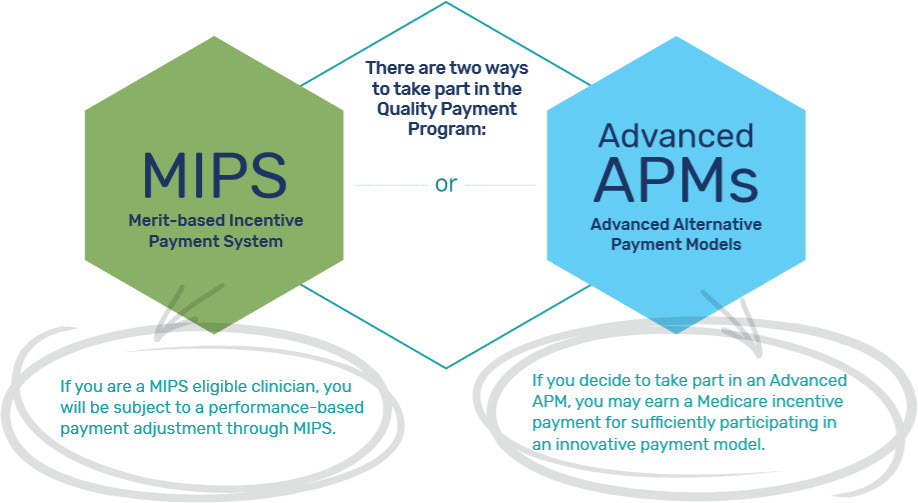
With MIPS, you may earn performance-based payment adjustments for your services to Medicare patients.
The APM is a customized payment approach developed by CMS, often designed to incentivize clinicians who provide high-quality, high-value care. APMs can focus on specific clinical conditions, care episodes, or populations.
MIPS Calculation for 2024
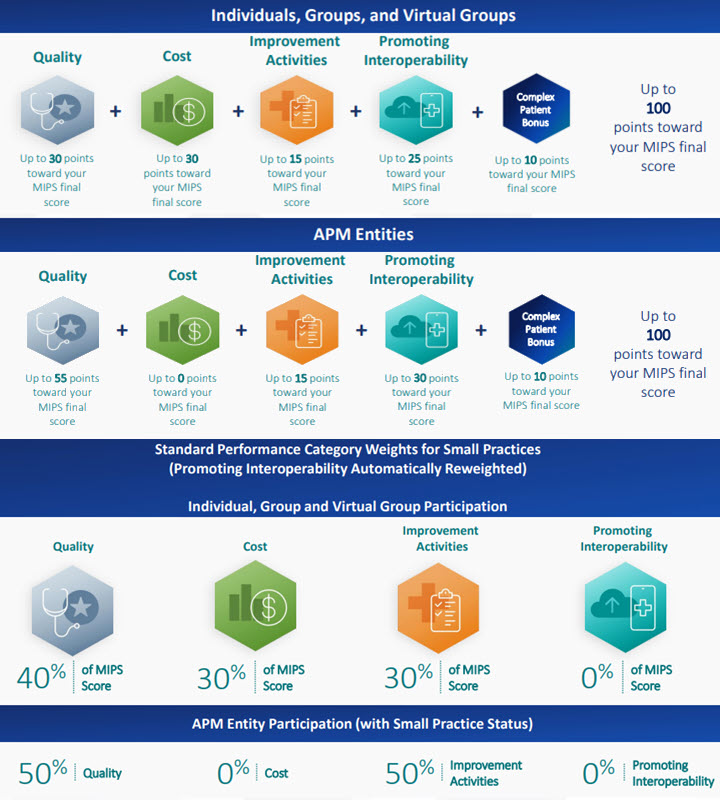
The MIPS score is based on four categories: Quality, Cost, Improvement Activities, and Promoting Interoperability.
The performance categories have different “weights,” and the scores are added together, resulting in a final MIPS Composite Performance Score (CPS).
A MIPS score is a number between 0 and 100 that measures the performance of Medicare Part B clinicians. The score determines the adjustment to a clinician’s Medicare Part B payment.
Penalties and rewards are distributed on a sliding scale based on how far below or above you score against the MIPS performance threshold set for that performance year.
Changes to the MIPS Program for Performance Year 2024
After five years, the special COVID hardship waiver has ended. In 2024, MIPS will be fully in force for all eligible clinicians across all specialties. A total of 198 quality measures were finalized for the 2024 performance period, resulting in the following changes:
- Removal of 11 quality measures
- Modification of 59 existing measures
- Addition of 11 new quality measures
With the push to transition to MIPS Value Pathways (MVPs), CMS has finalized five new MVPs and modified the previously 11 finalized MVPs.
There will be 16 MVPs available for reporting in the 2024 performance period. The identification of MIPS MVPs typically occurs after the performance year’s end and is based on various performance metrics and criteria set by CMS.
Point Thresholds
The performance threshold for the 2024 MIPS performance year will remain at 75 points. CMS proposed increasing the performance threshold to 82 points for the 2024 performance year, but this proposal was not finalized.
Data Completeness Threshold
CMS previously finalized an increase to the data threshold requirement. Now, 75% data completeness is required for the 2024 and 2025 performance periods (up from 70% in 2023) for all:
- eCQMs
- MIPS CQMs
- QCDR measures
- Medicare Part B claims measures
MVPs (MIPS Value Pathways) Changes
The number of available MVPs clinicians can report on has increased from 12 in 2023 to 16 in 2024.
Quality Category Changes
- In 2023, clinicians were required to achieve 70% data completeness for each quality measure. In 2024, you are required to achieve 75% data completeness.
- The number of available quality measures remains the same at 198, but modifications were made:
- Addition of 11 new quality measures
- Complete removal of 11 quality measures
- Partial removal of 3 quality measures (retained for MVP use only)
- Substantive changes to 58 existing quality measures.
Improvement Activities (IA) Category Changes
- The number of available Improvement Activities has increased from 104 in 2023 to 106 in 2024
- Addition of 5 new improvement activities
- Removal of 3 improvement activities
- Modification of 1 existing improvement activity
Promoting Interoperability (PI) Category Changes
- The performance period for the PI category has been changed from 90 continuous days in 2023 to 180 continuous days in 2024.
- Clinicians must now attest “yes” to the SAFER Guide measure.
- Automatic reweighting for the PI category has been altered for some clinician types, with some types being disqualified for reweighting and others gaining qualification. The following chart shows which types are being altered:
| Now Disqualified | Still Qualified |
|---|---|
| Physical Therapists | Clinical Social Workers |
| Occupational Therapists | ASC-Based Clinicians and Groups |
| Qualified Speech-Language Pathologists | Hospital-Based Clinicians and Groups |
| Clinical Pathologists | Non-Patient Facing Clinicians and Groups |
| Registered Dieticians or Nutrition Professionals | Clinicians in a Small Practice |
Cost Category Changes
- CMS is updating how they calculate the cost category for PY24 to match the quality category scoring methodology precisely.
- There will be a total of 29 Cost measures available in 2024, including the addition of 5 new episode-based measures.
With the many changes ahead, participants are urged to gain clarification to ensure how this impacts their reporting. Most at risk are the practices that utilized the COVID-19 Extreme and Uncontrollable Circumstance (EUC) hardship exception, which has expired.
Quality Performance Category
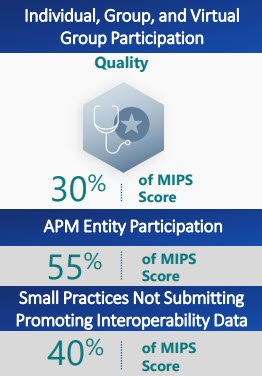
30% of final score
This percentage can change due to special statuses, exception applications, Alternative Payment Model (APM) Entity participation, or reweighting of other performance categories.
There are five collection types for MIPS quality measures:
- Electronic Clinical Quality Measures (eCQMs);
- MIPS Clinical Quality Measures (CQMs);
- Qualified Clinical Data Registry (QCDR) Measures;
- Medicare Part B Claims Measures; and
- The Consumer Assessment of Healthcare Providers and Systems (CAHPS) for MIPS Survey.
Reporting a measure that doesn’t meet the case minimum, data completeness, or a benchmark (historical or performance period) is unavailable will result in 0 out of 10 points (3 points for small practices).
You must collect and submit measure data for the 12-month performance period (January 1 – December 31, 2024).
Links to 2024 MIPS Quality Performance Documentation
- 2024 MIPS Quality Measures List (999KB XLSX)
- 2024 Cross-Cutting Quality Measures (294KB PDF)
- 2024 MIPS Clinical Quality Measure Specifications and Supporting Documents (58MB ZIP)
- 2024 Electronic Clinical Quality Measure (eCQM) Specifications
- 2024 Qualified Clinical Data Registry (QCDR) Measure Specifications (636KB XLXS)
- Small practices only: 2024 Medicare Part B Claims Measure Specifications and Supporting Documents (10MB ZIP)
- 2024 Acute Cardiovascular-Related Admission Rates for Patients with Heart Failure Measure (1MB ZIP)
- 2024 All-Cause Unplanned Admissions for Multiple Chronic Conditions Measures (5MB ZIP)
- 2024 All-Cause, Unplanned, Hospital-Wide Readmission Measure (822KB ZIP)
- 2024 Hip Arthroplasty and Knee Arthroplasty (THA/TKA) Complications Measure (568KB ZIP)
- MVP reporting only: 2024 MVP Quality Measure Specifications for Quality IDs 112, 113, 128 (2MB ZIP)
Promoting Interoperability (PI) Performance Category
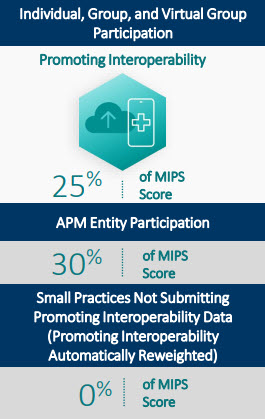
25% of final score
This percentage can change due to special statuses, an approved hardship exception application, Alternative Payment Model (APM) Entity participation, or reweighting of other performance categories.
Beginning with the 2024 performance period, you must submit collected data for required measures from each objective (unless an exclusion is claimed) and answer “yes” to all the necessary attestations for the same 180 continuous days (or more) during the calendar year.
Links to 2024 MIPS Promoting Interoperability Performance Documentation
Improvement Activities Performance Category
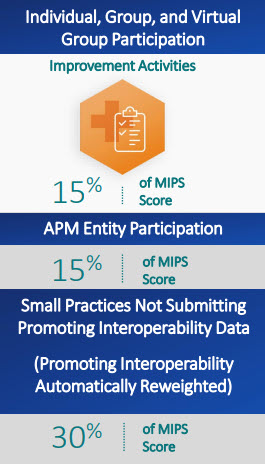
15% of final score
This percentage can change due to special statuses, exception applications, Alternative Payment Model (APM) Entity participation, or reweighting of other performance categories.
You must perform between 1 and 4 improvement activities depending on your reporting requirements.
Improvement activities have a continuous 90-day performance period (during the 2024 performance year) unless otherwise stated in the activity description below.
Links to 2024 MIPS Improvement Activities Performance Documentation
Cost Performance Category
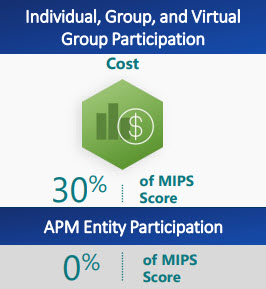
30% of final score
This percentage can change due to exception applications, Alternative Payment Model (APM) Entity participation, or reweighting of other performance categories.
There are 29 cost measures available for the 2024 performance period, including:
- Episode-based cost measures based on a range of procedures, acute inpatient medical conditions, chronic conditions, and
- Population-based cost measures focused more broadly on primary and inpatient care.
If you don’t meet the established case minimum for any available cost measures, the cost performance category will receive zero weight when calculating your final score. The 30% for this category will be distributed to another performance category (or categories).
You don’t need to submit data for the cost performance category. Cost measures are evaluated automatically through administrative claims data.
Links to 2024 MIPS Cost Performance Documentation
- 2024 MIPS Cost Measure Information Forms (47MB ZIP)
- 2024 MIPS Summary of Cost Measures (505KB PDF)
- 2024 MIPS Cost Measure Codes List (14MB ZIP)
Payment adjustments
The final score determines the payment adjustment, which can be negative, neutral, or positive:
Negative adjustment
A score of 0–18.75 points results in a negative adjustment of -9%. A score of 18.76–74.99 points results in a negative adjustment between -9% and 0%.
Neutral adjustment
A score of 75.00 points results in a neutral adjustment of 0%.
Positive adjustment
A 75.01–88.99 points score makes a positive adjustment but is subject to a scaling factor.
MIPS Data Collected
The Health Providers DB includes the following details from the MIPS database.
https://data.cms.gov/provider-data/dataset/a174-a962
| Name | Description |
|---|---|
| NPI | The unique clinician ID assigned by NPPES. |
| PAC ID | The unique group ID assigned by PECOS to the group this individual participated in. |
| Provider First Name | Individual clinician’s first name. |
| Provider Last Name | Individual clinician’s last name. |
| Source of scores | The method by which the clinician achieved scores (“individual”, “group”, “virtual group”, or “apm”); if the source is “apm”, this indicates that the MIPS APM scoring standard was applied for this set of scores. |
| Quality category score | Quality performance category score. |
| PI category score | Promoting Interoperability (PI) performance category score. |
| IA category score | Improvement Activities (IA) performance category score. |
| Cost category score | Cost performance category score. |
| MIPS Final Score without CPB | MIPS Final Score without the Complex Patient Bonus (CPB). The CPB is part of the MIPS final score based on the overall medical complexity and social risk for one’s patients treated. |
| MIPS Final Score | MIPS Final Score. |