HealthProviders DB profiles include State Terminations, Suspensions, Sanctions, and Exclusions, as Exact or Possible matches, greatly simplifying your exclusion research.
An individual or organization whose billing privileges have been revoked in any State cannot participate in Medicaid, Medicare, or the Children’s Health Insurance Program (CHIP).
Avoid potential Civil Monetary Penalties (CMPs) with HealthProviders DB Batch Exclusion Screening and Exclusion-monitoring Solutions.
Search HealthProviders DB
Exclusions are imported monthly as they become available and matched to the Providers’ Profile as Exact or Possible matches. Exclusions that match by NPI number, or by full name and address, are Exact matches.
Enter an NPI number, license number, or provider name in the search field below to search the Exclusions. Alternatively, you can also search the Providers. Remove the State filter to search all State Exclusion Lists, OIG Exclusions, SAM Debarments, FDA Debarments, and Clinical Investigators—Disqualification Proceedings—simultaneously!
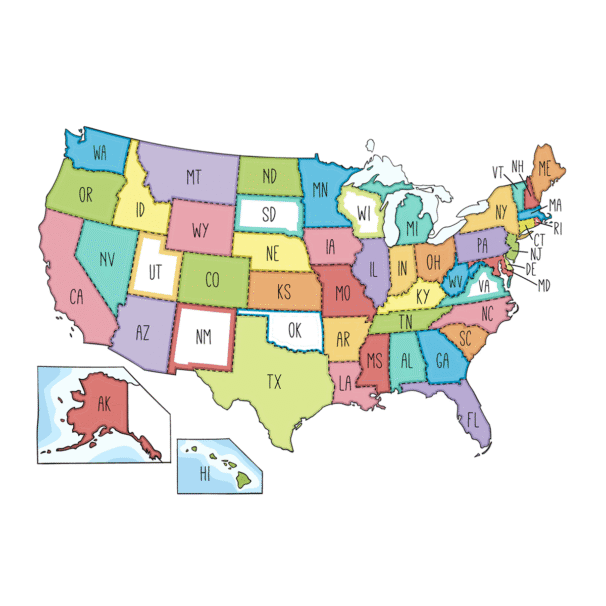
Select a State below to view the list of Exclusions by State. Additionally, you can narrow the list by city, among other options, from the Filter Panel, which you can open by clicking the vertical ellipses ⋮ in the upper right corner of the app.
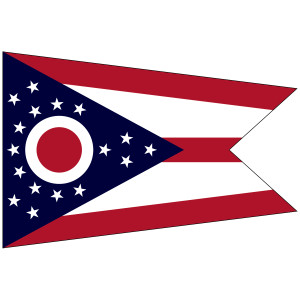
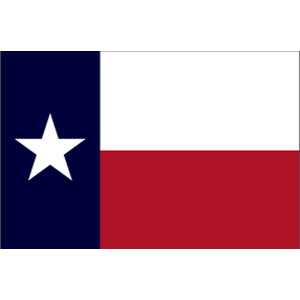
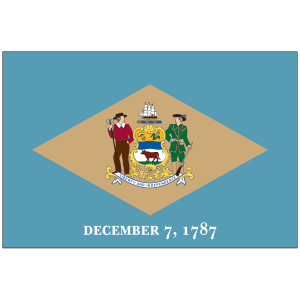
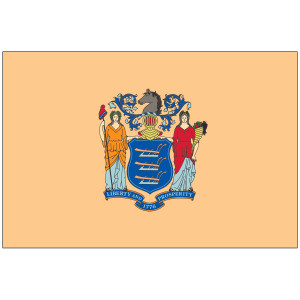
Alaska – Alabama – Armed Forces Pacific – Arkansas – American Samoa – Arizona – California – Colorado – Connecticut – District of Columbia – Delaware – Florida – Federated States of Micronesia – Georgia – Guam – Hawaii – Iowa – Idaho – Illinois – Indiana – Kansas – Kentucky – Louisiana – Massachusetts – Maryland – Maine – Marshall Islands – Michigan – Minnesota – Missouri – Northern Mariana Islands – Mississippi – Montana – North Carolina – North Dakota – Nebraska – New Hampshire – New Jersey – New Mexico – Nevada – New York – Ohio – Oklahoma – Oregon – Pennsylvania – Puerto Rico – Palau – Rhode Island – South Carolina – South Dakota – Tennessee – Texas – Utah – Virginia – Virgin Islands – Vermont – Washington – Wisconsin – West Virginia – Wyoming
State Exclusion Lists
Every State has a department or agency responsible for maintaining the integrity of its Medicaid programs and public health initiatives. While the names of these enforcement authorities may vary—such as the Department of Medicaid or the Department of Health Care Services—they all create regulations regarding the ineligibility of providers who have been disciplined or have lost specific licensing privileges.
State Lists vs. OIG LEIE
States are required to notify the Health and Human Services (HHS) Office of Inspector General (OIG) only when they exclude or terminate an individual or entity based on federal law.
They are not required to notify the OIG (nor should they) for terminations and exclusions based on State laws, because if the sanction fails to meet the criteria for a federal exclusion, it will not be included on the OIG List of Excluded Individuals/Entities (LEIE).
For instance, a State might exclude a party for failing to pay State taxes or for a variety of other reasons that would not be valid bases for federal exclusion. For this reason, states maintain a list of individuals and entities who are terminated, suspended, sanctioned, or otherwise excluded from the State Medicaid program under State law.
States may also maintain their lists as central registries for State sanctions, including non-healthcare actions and exclusions or terminations. For example, federal exclusions can be imposed for failing to repay federal loans, and it would be reasonable for a State to have a similar exclusion basis.
Unfortunately, each State that publishes an exclusion list has different formats and varying levels of detail. Some states provide only the name of the excluded individual or entity, along with a possible address and sometimes just a city.
States are not required to maintain a State exclusion list, and seven states have elected not to: New Mexico, Oklahoma, Rhode Island, South Dakota, Utah, Virginia, and Wisconsin.
This is a problem because, without a separate state-sanctioned or exclusion list, it is difficult to determine whether an individual or entity has been excluded or terminated under State law.
Arkansas


Colorado


Delaware

Illinois

Kentucky




Minnesota


Missouri

Nebraska

New Mexico






Rhode Island

South Dakota



Washington

Wisconsin